'Mild-course', home-isolated: still a missing puzzle to understand the COVID-19 pandemic
Since the last post (a while ago), many things happened: to the pandemic, which we can now effectively fight against, to the awakening world economy, the even warmer climate... But also to the blog author, who now pursuits a free-lance data scientist career (https://www.daas.tirol/) - any time happy to crunch your exciting data!
In the mean time, I spent days if not weeks with an extremely interesting project named simply 'Health after COVID-19 in Tyrol', whose results, while still not 'properly' published, can be accessed as a preprint. Well, probably there's probably no single person who hasn't heard the term 'long COVID', either from media, friends or relatives - a phenomenon of symptom persistence long after the acute SARS-CoV2 infection ranging from an isolated smell disorder to debilitating shortness of breath making everyday life a hard struggle.
Even though the condition follows the 'ebb and flow' pattern of broad public interest, the scientific and clinical knowledge about the prevalence, manifestations and recovery from acute and long COVID-19 bases on a handful of papers - with the most prominent and elegant app survey report by Carole Sudre and colleagues. For this reason, our not so small international Austria/Italy survey targeting the 'mild-course', somehow neglected population of home-isolated COVID-19 patients provides an important voice in the scientific debate on long COVID.
Recovery from 'mild' COVID-19 can be a tough process...
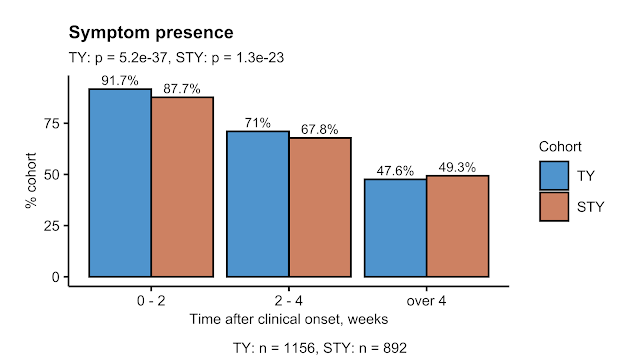
Not only for hospitalized cases as described by us previously. In the 'Health after COVID-19 in Tyrol' survey we asked primarily home-isolated people recovering from a laboratory confirmed SARS-CoV2 infection a series of questions concerning biometry, demographics, social status, medical history before the infection, symptoms and recovery status. Given that our target population encompassed only adult residents of Tyrol/Austria and South Tyrol/Alto Adige/Italy, we could reach over 2000 and 1000 participants from respective regions. If you consider 66K Tyrol SARS-CoV2 cases and 76K patients in the neighboring province since the pandemic onset, we could cover somehow 1.3 - 3% of the total regional convalescent population! In the analyses disclosed in our preprint, we focused on the population which may fall under the definition of long COVID, i. e. 28 days or longer with at least one symptom, by including only the respondents with an SARS-CoV2 test to study completion 'observation time' of 4 weeks or longer (Tyrol: n = 1157, South Tyrol: n = 893).
As you may appreciate above, we were quite surprised to see so many respondents (nearly 50%!) with at least one long-lasting complaint far beyond the the official duration of quarantine varying between 10 and 14 days on average. It has to be noticed, that these figures are placed at the upper limit of the range found in literature and are in part the consequence of a selection bias - a subset of not completely recovered COVID-19 patients responded to the survey invitation with a larger likelihood than people with a complete and instant recovery. You may also notice a minute fraction of the participants with asymptomatic infection, which speaks for such phenomenon. While this is a clear limitation of our study design, still we could learn a lot from these data: first of all that there's a non-negligible fraction of patients for whom a come-back to work, social and family life after 'mild' COVID-19 may be quite problematic.
Disease phenotypes: many faces of the disease
Most data professionals know from their experience that such conspicuous patterns are strongly 'data-driven' not to say ephemeral: once you take another set of observations, they're often gone. By saying that I don't want to discredit the usefulness and value of clustering analysis, a great tool for discovery of real, actionable data structures. In our study cohorts - differing in social structure, languages, containment management measures - the acute COVID-19 symptom phenotypes were nearly identical, suggesting that there are real biological processes behind the scenes... Speculatively, we might be able to capture two varieties of the same, officially 'mild' COVID-19 - a typical upper respiratory tract infection like many and a systemic condition attacking the lower airway, digestive tract and nervous system either via the virus or an exaggerated immune response to the pathogen.
For persistent symptoms contributing to long COVID, we could observe a quite different landscape of manifestations, last but not least due to rapid resolution of the 'flu-like' non-specific infection symptoms. While the MOP continued to exist in a fairly similar form, we could additionally dissect two 'minior' subsets of long-lasting sequelae: the fatigue and the hypo/anosmia phenotype (smell deficit or loss in clinical jargon).
Figure 3. Co-occurrence of long COVID complaints in symptomatic cases in the Tyrol cohort analyzed by PAM clustering. SMC: simple matching coefficient, MOP: multi-organ phenotype, FAP: fatigue phenotype, HAP: hypo/anosmia phenotype.
We could exploit this post-acute phenotype symptom burden to classify the long COVID participants. Despite the anecdotal knowledge, a smell or taste disorder does not seem to be an isolated or widespread complaint in the study subsets affected by long COVID. Instead, persistent fatigue, tiredness, brain fog, memory and concentration problems were present in the study populations to a substantial percent, i. e. complaints which may particularly hamper one's everyday performance. Interestingly, in the affected population, the subset suffering from either a smell or taste disorder was the 'beneficial' one with the lowest net count of persisting symptoms, neuro-cognitive manifestations and plagued by post-COVID fatigue to a lesser extent. Respondents with both the taste and smell disorder or, conversely, with those senses preserved, were much worse off.
Figure 4. Classification of the long COVID participants by DBSCAN clustering. Note the HAPint subset (either smell or taste disorder) with the lowest persistent symptom burden.
Who is at risk of long COVID?
Finally, with the limitations of the retrospective study design in mind, we dared to specify, who is at risk of developing long COVID. The condition was previously reported to be a predominantly female phenomenon linked to the burden of acute coronavirus infection defined as the symptom count. In addition, smell and/or taste disorders were put forward as 'warn signals' of the protracted recovery. To this end, we used LASSO, an enhanced form of the traditional linear modeling. Despite lots of formulas in the linked article it's a simple method in its principle that makes you find a minimal though decent set of factors associated with the risk - in this case of long COVID. The downside is that the approach, just like clustering, has a limited potential to explain general phenomena. Nevertheless, we our LASSO models fitted separately to each cohort's results, we could identify several common 'red flags' of the perturbed COVID-19 recovery: smell/taste disorders, shortness of breath, memory and cognitive disorders of acute SARS-CoV2 infection, hair loss and, not quite surprisingly, the observation time.
Figure 5. Risk factors of long COVID identified by LASSO regression in the Tyrol and South Tyrol cohort.
Importantly, acute memory problems and dizziness were flagship complaints of the multi-organ phenotype or MOP. Unexpectedly, the female sex didn't belong to this minimal set of risk factors. Possible explanations are sex and age weighting applied in our modeling approach and a differing profile of acute COVID-19 manifestations between the sexes - the topic of a current sub-project.
Take home message: even the 'mild' form of COVID-19 may have a systemic disease characteristic
The most important and novel finding of our 'both-Tyrol' study is the characteristic of the multi-organ form of mild COVID-19: not necessarily associated with respiratory problems but, additionally, with manifestations of the nervous, circulatory and gastrointenstinal system. Even though the exact, 'real-life' prevalence of such symptoms in the general of the convalescents still needs to be determined, we suggest that the group suffering from them is likely to experience complicated recovery, cognitive, mental and physical impairment and may require professional medical help.
References
- Sahanic S, Tymoszuk P, Ausserhofer D, et al. Phenotyping of acute and persistent COVID-19 features in the outpatient setting: exploratory analysis of an international cross-sectional online survey. medRxiv 2021; :2021.08.05.21261677. Available at: https://doi.org/10.1101/2021.08.05.21261677 - our recent long COVID-19 preprint
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med 2021; 27. Available at: https://pubmed.ncbi.nlm.nih.gov/33692530/ - the seminal app-survey long COVID-19 paper
- Blomberg B, Mohn KGI, Brokstad KA, et al. Long COVID in a prospective cohort of home-isolated patients. Nat Med 2021; Available at: https://pubmed.ncbi.nlm.nih.gov/34163090/- Bergen/Norway observation cohort study, a longitudinal characterization of long COVID
- Goërtz YMJ, Van Herck M, Delbressine JM, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res 2020; 6:00542–02020. Available at: https://pubmed.ncbi.nlm.nih.gov/33257910/
- Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021; :101019. Available at: https://pubmed.ncbi.nlm.nih.gov/34308300/







Comments
Post a Comment